Frequently Asked Questions
1. What factors can interfere with assessment of the Glasgow Coma Scale and what can be done about them?
Interfering Factors
There are three main sources of possible interference with assessment of one or more component of the scale.
- Pre-existing factors
- Language or cultural differences
- Intellectual or neurological deficit
- Hearing loss or speech impediment
-
Effects of current treatment
- Physical e.g. intubation or tracheostomy
- Pharmacological e.g. sedation or paralysis
-
Effects of other injuries or lesions
- Orbital/Cranial fracture
- Dysphasia or Hemiplegia
- Spinal cord damage
Actions to avoid loss of Information
- Communication Barriers:
Adapt the method of interaction to the patient, for example by choice of language, culturally appropriate examining person, or using written communication.
- Treatment influences
In the context of endotracheal intubation or tracheostomy, the verbal component of the score can be denoted as ‘not testable,’ NT. The motor and eye components can still be assessed and the trend will still be useful*.
For pharmacological impairment, temporarily reverse sedation and paralysis (wake up test)
- Other injuries
Adapt the examination technique for patients with spinal cord injury, for example by focusing on tongue and eye movements instead of hand movements
Correction of systemic hypoxia and hypertension will optimise the patient’s brain function.
*Dealing with missing information
There are various different strategies for dealing with information that is missing because of factors interfering with assessment such as those described above.
- Assess, communicate and make decisions using the remaining components. Although guidelines are often expressed in terms of a total GCS ‘score,’ the trend in whichever of the components (eye, motor or verbal) can be assessed is still valuable.
- Do not use number ‘1’ to record missing component; use ‘NT’ (Not testable).
- Do not report a total score when a component is Not Testable because the score will be low and this could be confusing to medical colleagues. This may also imply that the patient is more unwell than they actually are.
- It is possible using statistical methods to estimate a missing component from the findings in the other components. This is probably more relevant to research than clinical practice.
Meredith W, Rutledge R, Fakhry SM, Emery S, Kromhout-Schiro S. The conundrum of the Glasgow Coma Scale in intubated patients: a linear regression prediction of the Glasgow verbal score from the Glasgow eye and motor scores. J Trauma. 1998; 44:839-44; discussion 844-5.
2. How is the Glasgow Coma Scale modified for Children?
The scale can be applied without modification to children over 5 years old. In younger children and infants, an assessment of a verbal response as “orientated” and motor response as “obeys commands” is usually not possible. A ‘Paediatric Glasgow Coma Scale’ was therefore described in Adelaide in which responses were modified as below.
| Eye Opening | Verbal Response | Best Motor Response |
|---|---|---|
| Spontaneous | Talks normally | Obeys commands |
| To sound | Words | Localises pain |
| To pain | Vocal sounds | Flexion to pain |
| None | Cries | Extension to pain |
| None | None |
Although several other systems have been put forward, none has gained greater widespread acceptance. The findings on the Adelaide scale can be related to normal child development of response and to the total score to be anticipated at increasing ages.
| Verbal | Motor |
Expected Normal
Total Score |
|
|---|---|---|---|
| Birth | Cries | Flexion | 9 |
| 6 months | Vocal sounds | 10 | |
| 6-12 months | Localises | 11 | |
| 1-2 years | Words | 12 | |
| 2-5 years | Obeys | 13 | |
| >5 years | Orientated | 14 |
References
Simpson D Reilly P. Pediatric coma Scale. Lancet. 1982;450
Reilly PL, Simpson DA. Sprod R. Thomas L. Assessing the conscious level in infants and young children: a paediatric version of the Glasgow Coma Scale.Childs Nervous System. 4(1):30-3, 1988
Simpson DA. Cockington RA. Hanieh A. Raftos J. Reilly PL. Head injuries in infants and young children: the value of the Paediatric Coma Scale. Review of literature and report on a study.Childs Nervous System. 7(4):183-90, 1991
3. What is the reliability of the Glasgow Coma Scale? How is it optimised?
Consistency in its findings is a key feature of a clinical assessment and during the development of the Glasgow Coma scale it was shown to be better than existing methods.1 Although some subsequent studies reported levels ranging from very poor to excellent2 a definitive systematic review3 has shown that the reproducibility of the scale is usually high.
Variations in the methods and quality of the 52 studies reviewed precluded specification of a single overall figure for reliability. Nevertheless, 85% of the findings in the better studies showed substantial reliability as judged by the standard criterion of a kappa statistic (K) above 0.64 .Each of the components of the Scale was found to be highly reliable (K >0.6 in 89, 88 and 94 % for the eye, verbal and motor components respectively). The reliability of the sum score, although lower, was still substantial (K >0.6 in 77%). Doctors and nurses were found to use the Scale equally well.5
Reliability can be influenced by a number of factors, some potentially open to improvement, and the review pointed to clear benefits from training and education. Reliability was not influenced by diagnosis or treatment such as intubation, but estimates were lower in patients with moderate impairment of responsiveness.
Consistency in technique of assessment and clear criteria for assignment of responses enhance reliability.1 The widespread adoption of the scale has been accompanied a loss of standardization.6 The recommended modern structured approach7 aims to promote greater reliability by using a uniform approach based on allocation of ratings by defined criteria.
Reliability of the Scale is
- Substantial
- Higher than for the sum
- Score can be variable
Reliability is Improved by
- Training and education
- Use the Scale, not the Score
- Standardized approach
Bibliography
- Teasdale G, Knill-Jones R, van der Sande J. Observer variability in assessing impaired consciousness and coma. J Neurol Neurosurg Psychiatry. 1978;41(7):603-610.
- Baker M. Reviewing the application of the Glasgow Coma Scale: Does it have interrater reliability? Br J Neurosci Nurs. 2008;4(7):342-347. doi:10.12968/bjnn.2008.4.7.30674
- Reith FCM, Van den Brande R , Synnot A, Gruen R, Maas AIR. The reliability of the Glasgow Coma Scale: a systematic review. Intensive Care Med. 2016;42(1):3-15. doi:10.1007/s00134-015-4124-3
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174.
- Reith FC, Synnot A, van den Brande R, Gruen RL, Maas AI. Factors Influencing the Reliability of the Glasgow Coma Scale: A Systematic Review. Neurosurgery. 2017;80(6):829-839. doi:10.1093/neuros/nyw178
- Reith FCM, Brennan PM, Maas A, Teasdale GM. Lack of standardization in the use of the Glasgow Coma Scale. Results of international surveys. J Neurotrauma. May 2015. doi:10.1089/neu.2014.3843
- Teasdale G, Allan D, Brennan P, McElhinney E, Mackinnon L. Forty years on: updating the Glasgow Coma Scale. Nurs Times. 2014;110(42):12-16.
4. Is the Glasgow Coma Scale only for use in Head Injuries?
The Glasgow Coma Scale can be applied to describe impairment of consciousness from any cause. It has found most use in head injuries, but reports of its application in impaired consciousness from other aetiologies are indicated below. In conditions where the damage is predominantly focal, as in a stroke, additional information from assessment of the degree of any focal deficit is clearly important.
Spontaneous subrachnoid haemorrhage
Teasdale GM, Drake CG, Hunt W, et al. A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry. 1988; 51:1457
Spontaneous intracerebral haemorrhage
J. Claude Hemphill III,David C. Bonovich, Lavrentios Besmertis, Geoffrey T. Manley, S. Claiborne Johnston. The ICH Score A Simple, Reliable Grading Scale for Intracerebral Hemorrhage Stroke. 2001;32: 891-897
Ischaemic Stroke
C J Wier, A P J Bradford,K R Lees Ischaemic stroke The prognostic value of the components of the Glasgow Coma Scale following acute stroke Quarterly Journal of Medicine (2003) 96 (1): 67-74
Intracranial Infection and brain abscess
A prospective study of glasgow coma scale (GCS), age, CSF-neutrophil count, and CSF-protein and glucose levels as prognostic indicators in 100 adult patients with meningitis. C.-M. Schutte, C.H. van der Meyden. Journal of Infection 1998, Pages 112–115
Brain abscess in 142 patients: factors influencing outcome and mortality. Jen-Ho Tseng, Ming-Yuan Tseng. Surgical Neurology, 2006, Pages 557–562
General trauma
Early Physiologic Predictors of Injury Severity and Death in Blunt Multiple Trauma John H. Siegel, MD; Avraham I. Rivkind, MD; Samir Dalal, MD; Shirin Goodarzi, MS Arch Surg. 1990;125(4):498-508
Gennarelli TA, Champion HR, Copes WS, Sacco WJ. Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J Trauma. 1994; 37:962-8
Non traumatic coma
Nontraumatic Coma: Glasgow Coma Score and Coma Etiology as Predictors of 2-Week Outcome. Ralph L. Sacco, MD; R. VanGool, MD; J. P. Mohr, MD; W. A. Hauser, MD. Arch Neurol. 1990;47(11):1181-1184.
Comparison of APACHE II, MEES and Glasgow Coma Scale in patients with nontraumatic coma for prediction of mortalityŠtefek Grmec* and Vladimir Gašparovic† Critical Care 2001, 5:19–23
Poisoning
Reliability of the Glasgow Coma Scale for the emergency department evaluation of poisoned patients. K Heard, VS Bebarta - Human & experimental toxicology, 2004 197-200
5. When and how often should Observations be recorded?
The timing and frequency of assessment that are appropriate varies according to the stage after onset of the impairment of consciousness and the pattern in any previous observations of a patient. Observation should begin as soon as possible after onset of the impaired consciousness in order to guide initial management and to establish a baseline against which to interpret later findings. Observations initially should be repeated frequently to establish if the patient is stable or to detect any trends of improvement, or of deterioration from developing complications. When a stable pattern emerges as time passes, the frequency can be reduced.
Specific criteria for patients with an acute head injury have been suggested by NICE [1]:
| Frequency of observation | Observations should be performed and recorded on a half hourly basis until GCS equal to 15 has been achieved. If GCS=15 observe: half-hourly for 2 hours, then 1 hourly for 4 hours, then 2 hourly thereafter; Should the patient with GCS equal to 15 deteriorate at any time after the initial 2-hour period, observations should revert to half-hourly. |
|---|---|
| Urgent reappraisal by the supervising doctor |
A sustained (that is, for at least 30 minutes) drop of one point in GCS level (greater weight should be given to a drop of one point in the motor score of the GCS); Any drop of 3 or more points in the eye-opening or verbal response scores of the GCS or 2 or more points in the motor response. |
- NICE : National Institute of Clinical Excellence Clinical Guideline 176 Head Injury :Triage, Assessment, investigation and early management of head injury in children, young people and adults. 2014
6. How much change is important?
Rigid criteria for what changes should prompt actions are not appropriate; circumstances vary widely and the role of the scale is to support not replace clinical decision-making. Nevertheless, some factors can provide guidance.
If responsiveness reduces, the features to take into account in deciding action include:
- The pattern of responsiveness before the change: the more stable the pattern, the more a change may be important
- The level of responsiveness before the change: the lower the preceding responsiveness the sooner action is appropriate.
- The aspect of the scale that has changed and the extent of the change: motor changes usually call for a response sooner than changes to the eye or verbal components.
- If the change persists when assessment is repeated, including confirmation by a colleague if doubt remains, then the change is more likely to be significant.
7. What are the relationships and roles of the Coma Scale and the Coma Score?
Scale versus score
The core concept in the Scale is that the patient’s eye, verbal and motor responses are described in simple, objective terms in order to convey a clear unambiguous picture of their condition.1 The allocation of numbers to the steps in the three responses (e.g. E=3, V=4, M=5) was introduced later to facilitate entry of clinical findings into a databank.
The Glasgow Coma Scale Score is produced by adding the numeric values of the three responses into a sum or composite total (e.g. E3, V4, M5 = Score 12).2 The lowest Score possible is 3, indicating deep coma, and the highest Score is 15, indicating normal consciousness. The other 11 Scores can reflect 118 different combinations of the three responses. Not all of these are clinically realistic.
Although the Score was initially developed to summarise information about patient groups , it became widely used in clinical practice as a ‘shorthand’ way of communicating the severity of a patient’s condition. A widely used classification system stratifies the early severity of head injury into mild (sum score 13–15), moderate (sum score 9–12) and severe (sum score < 8).
Relation between the scale and the score
The contribution of the components of the Scale to the sum score depends on the severity of the patients’ condition (Figure).3 In mild head injury the motor score has reached its maximum ‘ceiling’ effect and changes in the Score result only from changes in verbal or eye responses; in moderate head injury the motor score has a stable value and in severe head injury changes in the sum Score reflect changes only in the motor score.
The findings in each component of the scale and of the sum score both relate to prognosis. Studies of a very large database of 54040 patients 3.showed definitively that taking account of the findings from the components separately yields more information than using only the sum Score. Furthermore, the importance of the components varies according to the sum score, the motor component contributing most information in severe injury, the eye and verbal in mild and moderate injuries.
These findings underline the importance of assessing a patient’s impaired consciousness by the three separate clinical responses.
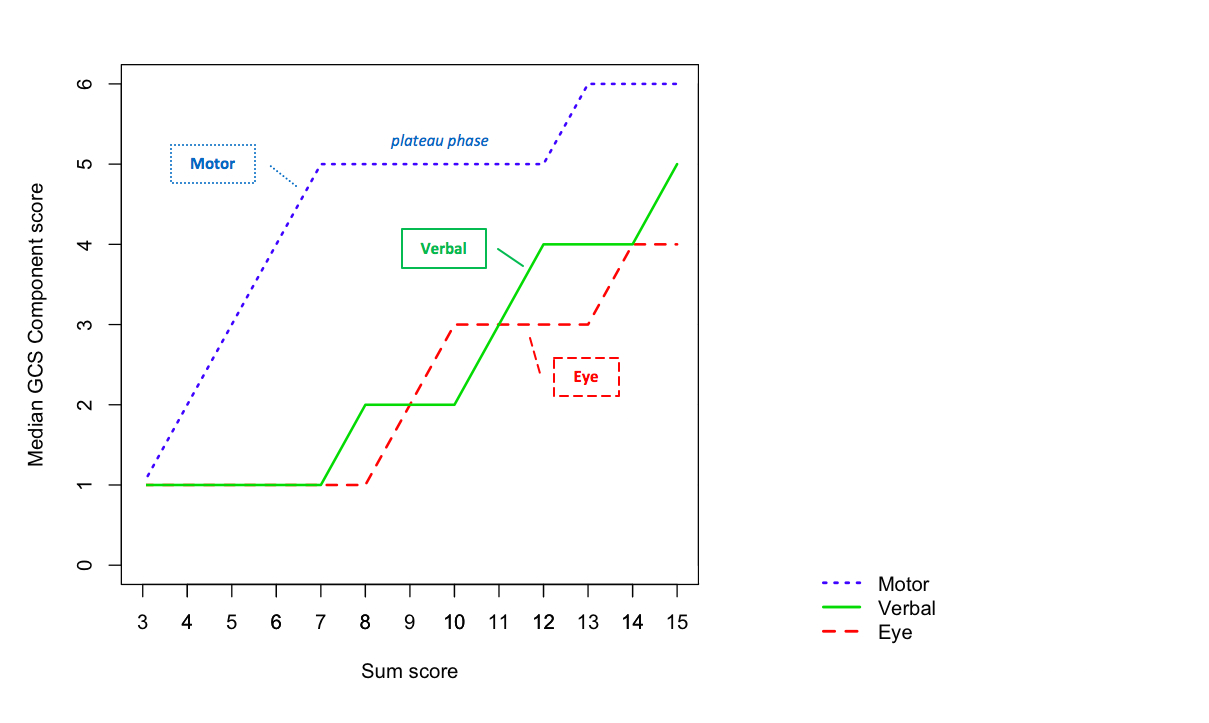
Figure showing the relation between the Scale and the Score
Clinical uses of the Score
The score is commonly used in the construction of clinical guidelines as produced by the Brain Trauma Foundation (severe TBI guidelines)4, the American College of Surgeons and Centers for Disease for control and prevention (National Trauma Triage Protocol)5 and the National Institute of Clinical Excellence (Head injury: assessment and early management NICE guideline)6 for decisions such as transport to a hospital, the need for a head CT, admission to the hospital, intubation, cervical immobilisation, undertaking surgery, and providing air transport.
The Score is included in many clinical stratification and severity prediction scores, such as Acute Physiology and Chronic Health Evaluation (APACHE) II7, Revised Trauma Score (RTS).8
It is a required component of the NIH Common Data Elements for studies of head injury.9
Recently the GCS Score and a pupil reactivity score have been combined into a new GCS-P score, with extended information about brainstem dysfunction (More information).10
Recommended practice in the use of the scale and score
The Score has limitations. It provides a less complete description of the patient than separate description of the three component responses of the scale. Also, the Score contains less prognostic information.3 Therefore, in clinical practice the three responses of the Scale should always be described rather than the sum Score alone.
In a minority of patients one or other of the components cannot be tested, usually the verbal response. In clinical monitoring this can be denoted by recording N T. This should not be translated into a value of 1 or zero in calculating a sum score. Methods for estimating the verbal response from the combined information from motor and eye responses have been described.11
Bibliography
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81-84.
- Teasdale G, Murray G, Parker L, Jennett B. Adding up the Glasgow Coma Score. Acta Neurochir Suppl. 1979;28:13-16.
- Reith FCM, Lingsma HF, Gabbe BJ, Lecky FE, Roberts I, Maas AIR. Differential effects of the Glasgow Coma Scale Score and its Components: An analysis of 54,069 patients with traumatic brain injury. Injury. 2017;48(9):1932-1943. doi:10.1016/j.injury.2017.05.038
- Carney N, Totten AM, OʼReilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. September 2016. doi:10.1227/NEU.0000000000001432
- Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep. 2012;61(RR-1):1-20.
- Davis T, Ings A, National Institute of Health and Care Excellence. Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults (NICE guideline CG 176). Arch Dis Child Educ Pract Ed. 2015;100(2):97-100. doi:10.1136/archdischild-2014-306797
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818-829.
- Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma Score. J Trauma. 1989;29(5):623-629.
- Grinnon ST, Miller K, Marler JR, et al. National Institute of Neurological Disorders and Stroke Common Data Element Project - approach and methods. Clin Trials Lond Engl. 2012;9(3):322-329. doi:10.1177/1740774512438980
- Brennan PM, Murray GD, Teasdale GM. Simplifying the use of prognostic information in traumatic brain injury. Part 1: The GCS-Pupils score: an extended index of clinical severity. J Neurosurg. 2018;128(6):1612-1620. doi:10.3171/2017.12.JNS172780
- Meredith W, Rutledge R, Fakhry SM, Emery S, Kromhout-Schiro S. The conundrum of the Glasgow Coma Scale in intubated patients: a linear regression prediction of the Glasgow verbal score from the Glasgow eye and motor scores. J Trauma. 1998;44(5):839-44; discussion 844.
8. What are the key references to development and use of the Glasgow Coma Scale?
The key references can be found here.